Impact Story
Neurotechnology for People: Dana and the Brain-Computer Interface Frontier
Jennifer French knows what it means to wait for technology to catch up with hope. For 25 years, she has lived with an implanted neuroprosthesis—a device that allows her to stand and transfer despite quadriplegic paralysis from a snowboarding accident in her early adult years. She’s witnessed firsthand the rare successes and what she calls the “copious failures” of neurotechnology devices trying to make it to market. She’s seen brilliant innovations die in what inventors grimly call the “Valley of Death,” that treacherous gap between laboratory triumph and real-world application.
“I’ve seen fantastic technologies do great things in the lab but fail in the marketplace,” says French, a Paralympic silver medalist who now directs the Neurotech Network. Her perspective, as both user and advocate, illuminates a fundamental challenge: How do we ensure that breakthrough brain-computer interfaces (BCIs) actually reach the people who need them?
It’s a question the Dana Foundation has grappled with for decades, and one that reflects a continuing evolution in the Foundation’s approach. From funding individual researchers with bold ideas about brain stimulation for depression to supporting collaborative communities that bring together patients, companies, regulators, and ethicists, Dana’s multi-decade commitment to neuroscience reveals a shift from asking “what is scientifically possible?” to “what is responsible and beneficial to people?”
A prime example of this evolution is brain-computer interface (BCI)—a range of technology that creates direct communication pathways between the brain and external devices, allowing signals from the brain to control computers or prosthetics, or enabling devices to modify brain activity.
Early Vision and Pioneering Support
The Dana Foundation’s support for brain-stimulation technologies began decades before the field went mainstream. Neurologist Helen Mayberg’s long-term relationship with the Foundation exemplifies this early vision.
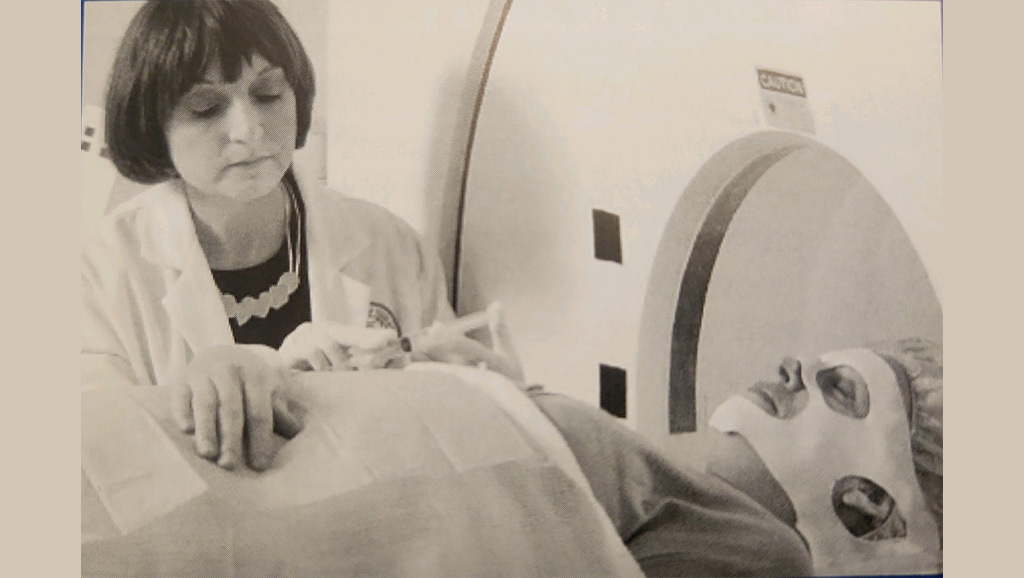
In 1995, Mayberg received a Clinical Hypothesis grant to test circuit-based models of mood regulation in patients with active and remitted depression, using PET scans—functional imaging that uses a tiny radioactive tracer to track brain metabolism. Years later, this basic science data proved foundational to a breakthrough clinical study using deep brain stimulation (DBS) to treat severe depression.
“Understanding the Circuits of the Brain” forum in Washington, D.C., 2007.
By 2007, Dana was funding an extension of Mayberg’s pioneering work using DBS—targeting electrical impulses to a specific part of the brain—for people whose depression had resisted every other therapy. The research had already shown promising early results in Toronto, where four of six patients experienced “a striking and sustained remission of depression.”
By the mid-2000s, the Foundation was supporting a growing number of researchers pushing the boundaries of brain stimulation as a potential treatment. In 2004, Peter Brown and Marwan Hariz received a grant to develop methods for Parkinson’s DBS surgery under anesthesia—work that would eventually help eliminate the need for patients to be awake during electrode placement.
That same spirit of innovation extended beyond neurology and psychiatry. In 2007, Kevin Tracey and his team tested whether externally stimulating the vagus nerve could calm the immune system and relieve symptoms in patients with intractable rheumatoid arthritis. This first-in-humans study—using a device that stimulated a branch of the vagus nerve through the ear—helped lay the groundwork for today’s rapidly advancing field of bioelectronic medicine, where neural circuits are harnessed to treat diseases far beyond the brain.
Dana also supported early work at the intersection of neuroscience, ethics, and society. Joseph Fins and Nicholas Schiff, with a 2003 grant, addressed one of medicine’s most profound challenges: understanding and potentially treating disorders of consciousness. They created basic ethical guidelines for undertaking experimental studies in minimally conscious patients. A second grant supported their efforts to build a scientific basis Ito distinguish among levels of minimal consciousness, helping predict who might benefit from DBS treatment. These frameworks have guided researchers, doctors, and families through decisions ranging from research participation to end-of-care planning.
This ethical foundation proved essential when, in 2007, Fins and Schiff made headlines with their DBS treatment of a 38-year-old man who had been minimally conscious since 1999. After DBS stimulation in the thalamus, he could communicate with gestures and short phrases, track people with his eyes, and eat independently. The transformation was remarkable, but the researchers knew it wouldn’t help everyone. These, and other cases, further refined their ability to identify which patients this treatment could help.
For Mayberg, currently the director of the Nash Family Center for Advanced Circuit Therapeutics at Mount Sinai, sustained Dana support proved transformative. Funding in 2007 helped establish the DBS lab at Emory University and supported both clinical trials as well as basic imaging studies to develop surgical targeting methods that use tractography, a 3D nerve-modeling technique now critical for optimizing treatment. A follow-up grant three years later provided early proof-of-principle for using DBS in mood disorders, using prototype devices that recorded neural oscillations even as they stimulated the brain.
“Dana funding allowed us to test high-risk hypotheses, not yet aligned with traditional NIH funding and prior to the establishment of the NIH BRAIN Initiative,” Mayberg says. “Dana funding enabled most of our most novel and impactful experiments over these many years.”
From Experimental Science to Collaborative Innovation
By 2010, this sustained support had established Dana as a crucial supporter of BCI pioneers. But as the field matured through the 2010s—with more than 12,000 people with Parkinson’s receiving deep-brain stimulators each year—the Foundation recognized it was time to pivot.
“In our early days of funding neuroscience and neurotechnology, we focused on the fundamental research to advance what was scientifically possible,” says Caroline Montojo, president of the Dana Foundation. “Fast forward to today, we’re shifting that focus to what is responsible and beneficial to people.”
This evolution is embodied in the Implantable Brain-Computer Interface Collaborative Community (iBCI-CC), launched in March 2024 with Dana support. Implantable BCIs—devices surgically placed in or on the brain to restore lost function or treat neurological conditions—represent some of the most advanced neurotechnology in development.
The collaborative model aims to build bridges across the “Valley of Death,” navigate regulatory hurdles, or achieve commercial viability. Leigh Hochberg, who directs the Center for Neurotechnology and Neurorecovery at Massachusetts General Hospital and also co-leads the iBCI-CC, has witnessed firsthand how researchers and companies with promising BCI technologies were struggling to reach patients.


iBCI-CC workgroup kickoff meeting. April 10, 2024. Photo courtesy of Jen French.
“Academic research has begun to pivot towards startup companies,” one step on the way to getting them to patients, Hochberg says. “But because these technologies are so novel, it’s been unclear how these devices would progress through regulatory processes and reimbursement discussions.”
A fundamental challenge: How do you measure whether a BCI actually works? Hochberg describes someone with ALS using an implanted BCI to communicate at 60 words per minute. “It may be super clear from a video that the technology is working and helping that individual achieve clinical outcomes that are important for them,” he says. “But 60 words per minute might not by itself be a clinical outcome measure that can be rigorously tested in a clinical trial.”
Without agreed-upon measures, companies can’t design trials that regulators will accept, and insurers won’t know what they’re paying for. It’s exactly the kind of problem that no single lab or company can solve alone.
Within months of forming, the iBCI-CC tackled this challenge head-on. Its Clinical Study Endpoints workgroup created the first comprehensive matrix of patient-centered outcome measures for implantable BCIs—developed through consensus among companies that will eventually compete, regulators who will evaluate their devices, and patients who will use them.
“This is the perfect time to be doing this,” Hochberg says. “Many of these trials are just getting off the ground. Some of them will launch in the next year or two.” The collaborative community provides “a place for easy, regular, transparent discussion” among all stakeholders.
“Dana knows neuroscience—and neuroethics,” Hochberg says. “The Dana executive team, the Dana board, they understand how advances can impact society, and how society can inform those advances.”
Another collaborative approach Dana is supporting is the American Brain Coalition’s partnership with the FDA’s Total Product Life Cycle Advisory Program (TAP). The TAP partnership tackles a specific challenge: The FDA has been eager to engage with patient communities, but the conversations needed to happen early in the device development process, not at the last, regulatory, stage.
Under the new partnership, the American Brain Coalition serves as “a translator and connector across the brain health community, industry, and government,” bringing patient groups ranging from Alzheimer’s to ALS to Parkinson’s disease into the conversations as early as possible.
“When people see their perspectives shaping device design and policy, it strengthens confidence in the entire system,” Montojo says. “This is especially important for technologies that interact directly with the brain.”
This shift from funding individual research to facilitating entire ecosystems reflects both the field’s maturation and Dana’s evolution.
As Mayberg observed: “Over my career, Dana has always been a presence—catalyzing pilot research projects, facilitating neuroscience outreach and education, encouraging societal and neuroethics discussions, enabling neuroscience networking.” What remained consistent was what Mayberg calls Dana’s “secret sauce”—a talent for creating connections among researchers that has now expanded to building bridges across many sectors of academia and society.
Looking Forward: From Innovation to Trust
As the Dana Foundation marks its 75th anniversary, its vision extends beyond the laboratory. “We envision a world where neurotechnology is both innovative and trusted,” says Montojo. “Our mission is to advance neuroscience that benefits society and reflects the aspirations of all people.”
This isn’t just aspirational—it’s taking concrete form. Students see themselves in neuroscience careers because they can see how it affects their lives. Student scientists are being trained to consider ethical and societal implications of their research. And models of doing science and building innovative devices are emerging where “community needs, priorities and values are reflected in the neuroscience enterprise.” Montojo says.
For Jennifer French, who has watched the field evolve for decades and is now co-lead of the iBCI-CC with Hochberg, Joe Lennerz, and Jessica Kelemen, the collaborative model offers hope that this generation of devices might actually cross the Valley of Death.
“We’re at a pivotal moment,” French says, “moving from first-in-human safety studies to making devices available on the market.” The difference now is that the people who will use these devices have a seat at the table from the beginning.
“The real credit goes to the extraordinary people who participate in clinical trials,” says Hochberg. But ensuring their sacrifices lead to accessible treatments requires the kind of ecosystem the Dana Foundation is helping to build—one where a matrix of outcome measures can guide trials, where regulators hear directly from patients, and where companies collaborate before they compete.
Dana’s evolution from funding individual neuroscience pioneers to catalyzing the conversations that shape how neurotechnology develops reflects the fundamental insight: The most complex challenges in neuroscience require collaboration across traditional boundaries.



